June 2019
INTERESTING ECG OF THE MONTH
Case History
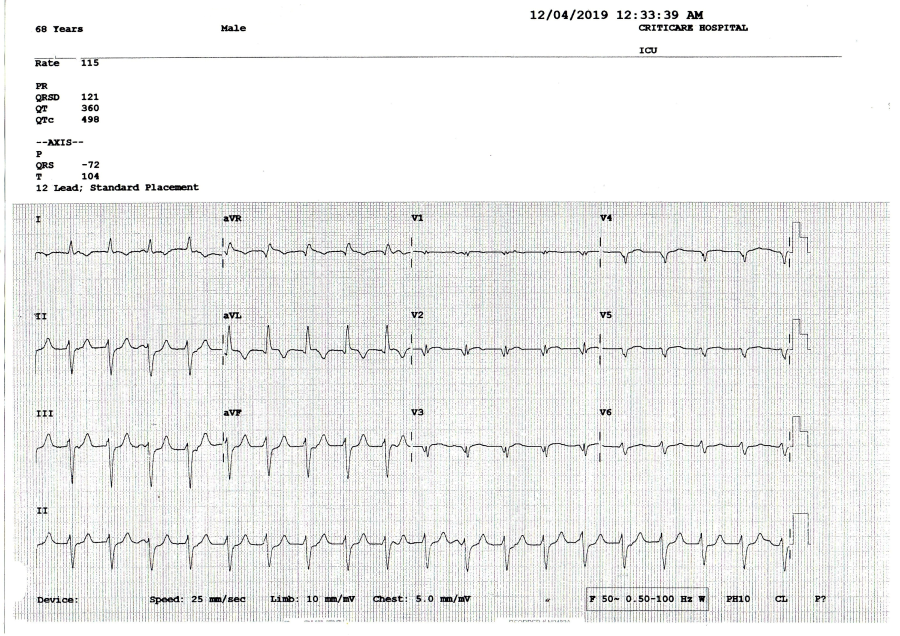
68 yrs old male with a past history of anterior wall myocardial infarction presented with recent onset shortness of breath.
Clinically he was stable; with systolic BP of 90/-.
His ECG shows tachycardia @ 110/m. What is the diagnosis?
The ECG shows tachycardia with a QRS width of 120 ms; left axis deviation & the precordial leads show poor progression of R wave. On careful evaluation there is evidence of AV dissociation in the long lead II & also there is a qr pattern in V2-V3. This confirms the diagnosis of slow VT.
Important to realize that VTs can be slow, hemodynamically tolerated and have a relatively narrow QRS. Past h/o AWMI should make one suspect any wide QRS tachycardia to be a VT.
INTERESTING ECHO OF THE MONTH
Case History
A 34 yrs female with a recent history of CVA and no other risk factors, was referred for Trans-oesophageal Echocardiography to rule out cardio embolic stroke. Her Contrast Trans-oesophageal Echo (TEE) was performed. What is the Diagnosis??
Her contrast TEE with valsalva maneuver showed contrast of agitated saline coming from SVC and opacifying the right atrium (RA). Subsequently there is a passage of these bubbles from RA to left atrium suggesting presence of a patent foramen ovale (PFO) with a significant right to left shunt. Presence of PFO is implicated in the etiology of cryptogenic stroke.
