Arrhythmia, Electrophysiology Study & Radiofrequency Ablation
February 11, 2019How Does The Normal Heart Work?
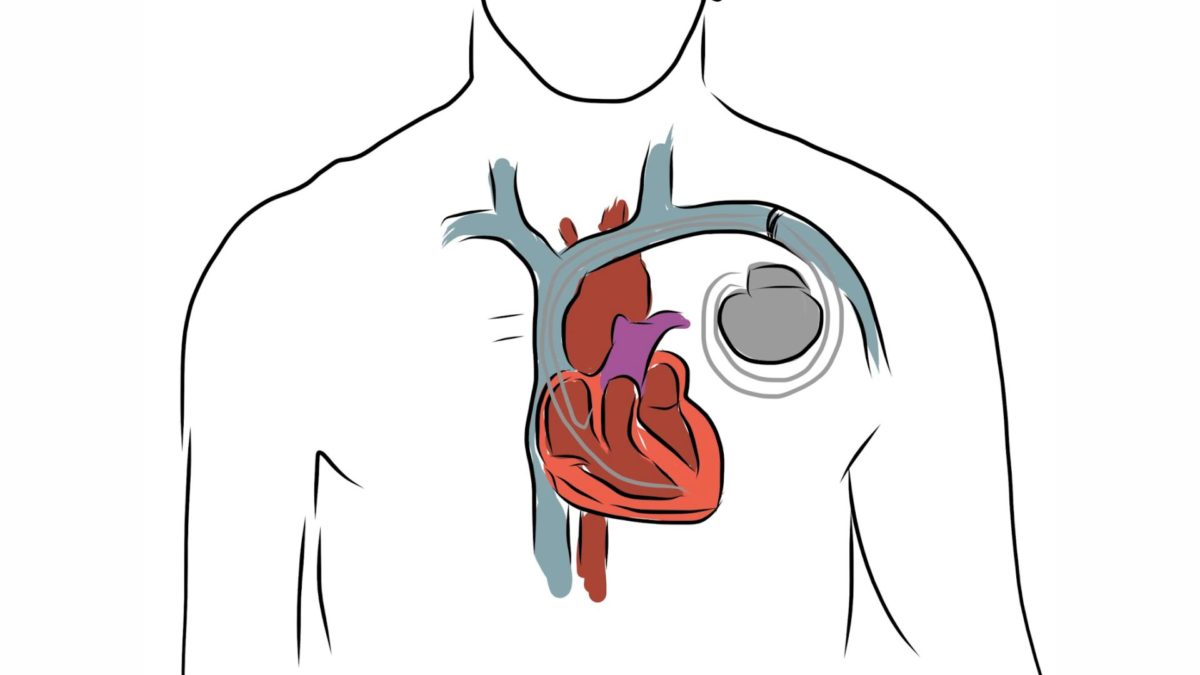
The human heart is an amazing pump. It has four chambers: two smaller, upper chambers called the right and left atria, and two larger, lower chambers called the right and left ventricles (refer to figure 1.0). These four chambers work together to produce powerful contractions (heartbeats) to constantly pump oxygen and nutrient – rich blood to your entire body.
The steady rhythmic contraction of your heart is controlled by the heart’s own electrical conduction system. Normally, the electrical signal to start a heart beat beings in the sinoatrial (SA) node located in the right atrium. The SA node is the natural pacemaker of the heart to beat regularly. Each pulse travels through the atria, causing them to contract, and then to a junction in the middle of the heart called the Atrioventricular or AV node.
The AV node is the only pathway available for the electrical pulses to travel from the atria to the ventricles. The pulse crosses the AV node and continues through the conduction pathways in the ventricles, causing them to contract and the heart to beat. After each beat the heart rests until the next electrical pulse from the SA Node begins the cycle again.
Normally, when you are at rest, your body’s blood and oxygen requirements are less and your SA node sends out impulses at a rate that causes your heart to beat between 60 to 80 times every minute. When you perform moderate physical exertion, the SA node increases your heart rate to about 100 beats per minute. During sustained strenuous exertion, your heart rate can rise up to 150 or more beats per minute to meet the high blood and oxygen demand of your body’s organs.
What Are Arrhythmias?
An abnormal heart rhythm that arises due irregularities in the heart’s electrical conduction system and associated tissues is called an arrhythmia or heart rhythm disorder.
During an arrhythmia the heart rate may be abnormally slow or abnormally fast or the heart’s rhythm may become abnormally irregular.
Abnormally slow heart rhythms (usually rates below 50 beats per minute) are known as Bradycardia. They usually occur due to defects in the SA Node or the AV Node. Bradycardia is very effectively treated by implantable pacemakers. These are electrical devices that artificially stimulate the heart and prevent it from beating too slowly.
Abnormally fast heart rates (usually 150 or more beats per minute) are known as Tachycardia. These are divided into two categories. Fast heart rates that begin in the upper chambers, the atria, are called Atrial Tachycardia. Fast heart rates that begin in the ventricles are called Ventricular Tachycardia (VT).
Although many types of arrhythmias are harmless, others can be extremely dangerous, even fatal. Therefore, it is important to determine the type of arrhythmia you have, establish how serious it is and begin appropriate treatment for your arrhythmia.
What Is Ventricular Tachycardia And Ventricular Fibrillation?
Fast rhythms beginning in your ventricles are called Ventricular Tachycardia (VT), the ventricular contractions are fast but regular and the heart may beat as fast as 200-400 beats per minute. VT often causes your ventricles to lose their pumping efficiency and could result in insufficient blood being pumped by the heart to your brain and other organs. As a result symptoms like palpitation, dizziness, shortness of breath and even loss of consciousness can occur.
VTs may occur in individuals who have heart diseases like:
- Blockages in the arteries (coronary artery disease)
- A previous heart attack (myocardial infarction)
- Heart muscle problems that cause the ventricles to dilate (dilated cardiomypathy) or the ventricular walls to become excessively thick (hypertrophic cardiomyopathy) heart failure (where the heart’s pumping efficiency is very poor)
Less frequently, VT can occur from rare inherited heart defects (long QT syndrome etc.), or even unknown causes. Ventricular tachycardia can be dangerous, even life-threatening if not properly treated.
At times, regular VT can degenerate into a completely irregular, unstable and chaotic electrical activity wandering around randomly in the ventricles. As a result, instead of contracting, the ventricles just quiver ineffectively and no blood is pumped by the heart to the brain and other organs, including the heart itself. This quivering of the ventricles as a result of chaotic electrical activity is called Ventricular Fibrillation (VF). The patient loses consciousness immediately after the commencement of VF and death occurs within minutes unless life-saving therapy is administered to the heart.
What Is Sudden Cardiac Arrest?
Sudden Cardiac Arrest (SCA) is the sudden, abrupt cessation of pumping of blood by the heart leading to immediate loss of consciousness and death.
The most common cause of SCA is ventricular tachycardia and ventricular fibrillation. SCA can occur without any warning and if the patient is to have any chance of survival he or she must be treated with a defibrillation shock within about six minutes.
Defibrillation is a technique in which a brief high-energy electric shock is administrated to the heart to treat life-threatening arrhythmias. The therapy can be given externally across the patient’s chest using an external defibrillator or internally using an implantable defibrillator. The shock passes through the heart, stops the erratic electrical activity that caused the cardiac arrest and allows the heart to return to a more regular rhythm.
Cardiac arrest is different from a heart attack. During a heart attack, the blood flow to portions of heart muscle is interrupted due to blockages in the arteries that supply blood to the heart muscle. These portions of heart muscle are therefore deprived of oxygen and get damaged or even die. Usually, however, the rest of the heart muscle still functions properly and the patient’s heart continues to pump blood, unlike during cardiac arrest.
Which Patients Are At A High-Risk Of Dying From Sudden Cardaic Arrest?
Since the most common cause of SCA is VT or VF, patient’s who have already experienced VT or VF or whose heart condition makes them vulnerable to developing VT or VF are at the highest risk of suffering from the SCA.
Various clinical studies that have studied patient risk for VT/VF and SCA suggest that the following groups of people are at highest risk for SCA:
- Patients who have already suffered an episode of SCA due to VF but who managed to survive.
- Patients with low heart pumping efficiency (indicated by a parameter called the ejection fraction) who have episodes of VT, especially when these episodes are associated with symptoms like dizziness and fainting
Patients who have episodes of VT but do not experience serious symptoms during these episodes could also be at high-risk and need to be further evaluated and suitably treated.
Patients who have suffered a heart attack and who have a poor heart pumping efficiency and whose heart possesses the triggers for causing VT / VF could also be at high risk for SCA. They must be carefully evaluated and suitably treated.
In addition to the above, patients who have dilated hearts (dilated cardiomyopathy) coupled with low heart pumping efficiency or heart failure, patients with abnormally thick ventricular muscle (hypertrophic cardiomyopathy) and some other structural heart problems could also be at high risk for SCA due to VT/VF. These patients too must be closely evaluated and suitably treated.
What Therapies Are Available To Manage Patients At High Risk For Sca?
Until the mid-1980s, ventricular tachycardia was treated mainly with medications. These medications work by reducing the frequency of occurrence of VT/VF and in this way attempt to prevent SCA. While these drugs do reduce the frequency of VT or VF, clinical studies have shown that in very high-risk groups of patient the best drugs available today are only partially effective in preventing SCA. Moreover, some of these drugs can have serious side-effects and studies have shown that up to 40% of patients do not take their medications regularly. All the same drugs continue to play a vital role in the management of patients with ventricular tachycardia. They are often used in conjunction with the other treatment options available for the management of SCA.
Radiofrequency ablation (or burning) is emerging as another treatment option for VT. This involves the insertion of soft, thin tubes called catheters into the heart through a vein. Once inside, these catheters are used to deliver energy to small portions of heart tissue that are responsible for starting or maintaining the VT. The energy heats up and destroys this portion of heart tissue and thereby prevents the VT from recurring. With the currently available technology, radio-frequency ablation has been successful in the treatment of very few types of VTs and is not yet a suitable treatment for the vast majority of VTs encountered.
Another way to treat VT/VF and prevent SCA is with a device called an Implantable Cardioverter Defibrillator (ICD).
What Is An Icd?
An ICD is a device that is implanted inside your body to treat VT/VF and thereby prevent Sudden Cardiac Arrest (SCA).
It works automatically by constantly monitoring your heart rate and detecting VT or VF episodes as soon as they begin. When an ICD detects an episode of VT or VF it immediately delivers therapy in the form of low energy electrical pulses or electric shocks to terminate the arrhythmias before they can harm the patient.
The ICD is a part of a system that has two main components – the ICD itself and the leads. The ICD is made of titanium metal and contains a battery, a microprocessor (a small computer) and electronic circuitry.
The leads are insulated wires that are threaded through a vein from the ICD to the inside of your heart. They serve to carry electrical signals from the heart to the ICD enabling the ICD to constantly monitor your heart rate and identify VT / VF episodes when they occur. The leads also serve to carry electrical impulses and shocks from the ICD to the heart to terminate VT/VF.
Today’s ICDs are capable of providing four types of therapies that can be performed by your doctor:
- Antitachycardia Pacing: In this type of therapy the ICD sends out bursts of low energy electrical pulses at a rate faster than the patient’s VT. For up to 95 % of VT’s, these rapid pulses are sufficient to terminate the VT. Most patients do not even feel these low energy pulses.
- Cardioversion Shock: If antitachycardia pacing does not stop the VT, the ICD can be programmed to deliver stronger electrical impulses called cardioversion shocks. These shocks may be programmed from low energy to high energy, as needed. Patients often describe the cardioversion shock as a thump on the chest and associate it with some discomfort.
- Defibrillation: If the ICD detects VF, it will send a high-energy shock to the heart to restore the heart to its natural rhythm. Some people lose consciousness when their heart goes into VF, so they are not aware of receiving the shock. Others who are awake during a defibrillation shock describe it as a “strong kick in the chest” that “passes very quickly”. Most of the time the realization that the shock has saved their life more than compensates for the discomfort patients feel from it.
- Bradycardia Pacing: If the ICD detects a very slow heart rate (bradycardia), it will pace the heart with electrical stimuli and prevent it from beating too slowly.
How Effective Are Icds?
The ICD was invented more than two decades ago with the specific purpose of automatically detecting and terminating life-threatening arrhythmias that cause Sudden Cardiac Arrest (SCA). Today, they are considered the most effective therapy available for the treatment of patients who are at high-risk for SCA due to VT/VF. The electrical therapies provided by ICD are up to 99% effective in terminating VT and VF.
Clear proof of the superiority of ICDs in preventing SCA over the currently available medicines for arrhythmia management has emerged from a number of clinical trials. Based on these trials, expert committees across the world have recommended ICD therapy in preference to other therapies in patients who are at high-risk of suffering from SCA due to VT/VF. On an average, patients who receive ICD therapy are likely to live significantly longer than those who are managed solely with medications.
Approximately 200,000 ICDs are being implanted per year worldwide (2004) and the number of implants is growing at a rapid rate.
How Is An Icd Implanted?
The ICD implant operation is not an open-heart surgical procedure. In fact, it is a relatively simple procedure that is performed under local anaesthesia and usually takes about 2 hours.
The ICD is usually implanted under the skin, in the left (and rarely in the right) chest area, just below the collar bone. The ICD leads are inserted into one of the veins located in the chest area that lead into the heart. The leads are pushed through these veins until they enter the heart and make contact with the heart tissue. The other end of the leads is inserted into the ICD.
Once the leads have been placed and connected to the ICD, the ICD system’s function is tested to ensure that it can effectively detect and terminate dangerous ventricular arrhythmias.
Patients are usually discharged from the hospital within 2 to 5 days after the ICD is implanted.
What Type Of Lifestyles Do Icd Patients Typically Lead?
Upon the advice of their physician, ICD patients can lead normal lifestyles which include:
- Pursuing hobbies or recreational activities
- Returning to their jobs
- Resuming strenuous activity
- Resuming sexual activity
- Travelling
Depending on the patient’s condition, the doctor may recommend avoiding situations where a few seconds of unconsciousness due to a rapid heart rhythm could be dangerous to the patient or others. Such activities may include driving, swimming, working with heavy machinery etc.
Patients with ICDs can safely operate both home and office electrical appliances.
ICD patients must strictly adhere to the routine follow-up schedule established by their doctor. In addition, when a patient feels symptoms or receives a shock, the patient must contact his or her physician.